General medicine Short Case
9 Feb 2022
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CHIEF COMPLAINT:-
A 19 years old male,student by the occupation presented to the opd with the chief complaints of vomitings 2-3 episodes since 3 days, abdominal pain since 3days and loose stools 4-5 episodes since 3days.
HISTORY OF PRESENT ILLNESS:-
Patient was apparently aymptomatic 3days back. Then he went to the function on one day and ate Mutton and oil rice. From then he developed pain in the abdomen which was sudden in onset, continuous in Nature and pain radiated to the left lower abdomen. vomitings 3-4 episodes per day, non-bilious , non-projectile,food as content. Then went to the local hospital.
PAST HISTORY:-
History of Hypertension and on regular medication since 2 years . No history DM,Asthma, epilepsy ,TB,CAD.
FAMILY HISTORY:- Not significant.
PERSONAL HISTORY:
Diet: mixed
Appetite : normal
Bowel and bladder : loose stools
Sleep :adequate
No addictions
No known allergies.
GENERAL EXAMINATION:-
Patient is conscious, coherent, cooperative and well oriented to time and place.
No pallor, cyanosis, icterus, clubbing, generalized lymphadenopathy.
VITALS:-
Temp: Afebrile
Pulse rate:- 86bpm
Respiratory rate:- 17breaths per min.
B.P:- 110/80 mmhg.
SYSTEMIC EXAMINATION:-
CVS-:-
S1 ,S2 sounds heard
No murmurs
RESPIRATORY SYSTEM:-
Bilateral air entry normal
No dypnea
No wheeze
Position of trachea-central
Vesicular breath sounds heard
ABDOMEN:-
Shape of abdomen -obese
Mild tenderness is present
No palpable mass
No bruit
CNS:-
Speech -Normal
No neck stiffness
No neurological deficits
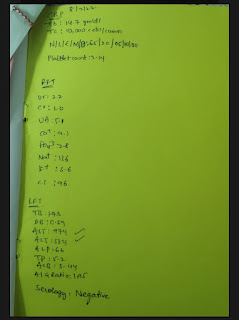
INVESTIGATIONS:-
CBP :-
Hemoglobin -14.7 gm/dl
TLC -10,000cells /cumm
Platelet count -2.14 lakhs
PROVISIONAL DAIGNOSIS:-
Acute Gasteroentiritis
TREATMENT:-
Inj PAN40 mg IV /stat
Inj ZOFER4mg IV/stat
Inj Metronidazole100 ml IV /stat
Tab Sporlac 2mg tab









Comments
Post a Comment